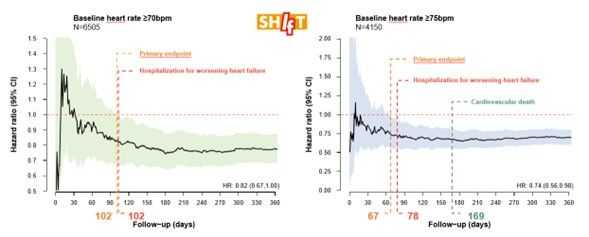
Time to benefit of heart rate reduction
Time to benefit of heart rate reduction with ivabradine in patients with HFrEF
In HFrEF, HR represents a modifiable risk factor associated with hospitalization and death. In addition, HR reduction with β-Blockers and ivabradine differed when HR remains above 70 bpm and particularly above 75 bpm despite β-Blocker treatment. Contemporary guidelines recommend an early start followed by up-titration of guideline-recommended HF drugs. However, current GDMT, such as sodium–glucose cotransporter 2 (SGLT2) inhibitors, angiotensin receptor–neprilysin inhibitors but also angiotensin-converting enzyme inhibitors and mineralocorticoid receptor antagonists have a lack HR reducing effects despite of significant therapeutic effects.
An analysis of early onset effects is not available for HR reduction with ivabradine. This is why the authors investigated a post-hoc analysis from SHIFT, exploring the composite of cardiovascular death and HF hospitalization and the components of the composite continuously according to treatment time.
This analysis reinforces the positive effect on CV death and HF hospitalization by HR reduction with ivabradine and showing a significant effect when considered for early initiation. HR reduction in heart failure should not be deferred, particularly in patients ≥ 75bpm: for the reduction of HF hospitalization, the treatment should be started early to achieve significant treatment effects at < 3 months for HR ≥75 bpm, and approximately 5 months for HR ≥70 bpm
Figure 1: Time to benefit of ivabradine in patients with HFrEF: analysis from the SHIFT study
For more information, : click here
HFrEF, Heart failure with reduced ejection fraction; HR, Heart rate; bpm, beats per minute; GDMT, Guideline-directed medical therapy; Reference: Michael Böhm et al. European Journal of Heart Failure (2023). doi:10.1002/ejhf.2870

Keep up to date with our content
Subscribe to our newsletter so that you are always up to date with the news.